Blog

St. Luke’s introduces individualized approach to breast cancer screening.
“When we look back on this time in future years, the hallmark of this era should not be that women stopped getting mammograms, but rather that this was a time when “personalized” screening strategies and technologies were provided to women, offering powerful weapons and options in the battle against breast cancer that were not available to their mothers and grandmothers.” -Joseph P. Russo M.D., section chief of St. Luke’s Women’s Imaging and director of the St. Luke’s Regional Breast Center.
When he was in high school, Dr. Russo lost his grandmother to breast cancer. Recently, another family member’s breast cancer was detected early, and as a result, she’s very much alive. Dr. Russo isn’t pleased about recent negative media coverage concerning life-saving mammograms.
“As radiologists, we’re aware of the limitations of mammography,” Dr. Russo says, “but more aware of the lives mammography has saved by detecting small, treatable breast cancers. A recent highly publicized Canadian study on mammography in the British Medical Journal (BMJ), unfairly, may have the negative effect of dissuading women from coming in for a mammogram. The truth is that studies still prove a 35% reduction in breast cancer mortality with routine screening mammograms. In addition, we are energized by the possibilities that new technologies offer.”
Breast screening, now personalized for the patient.
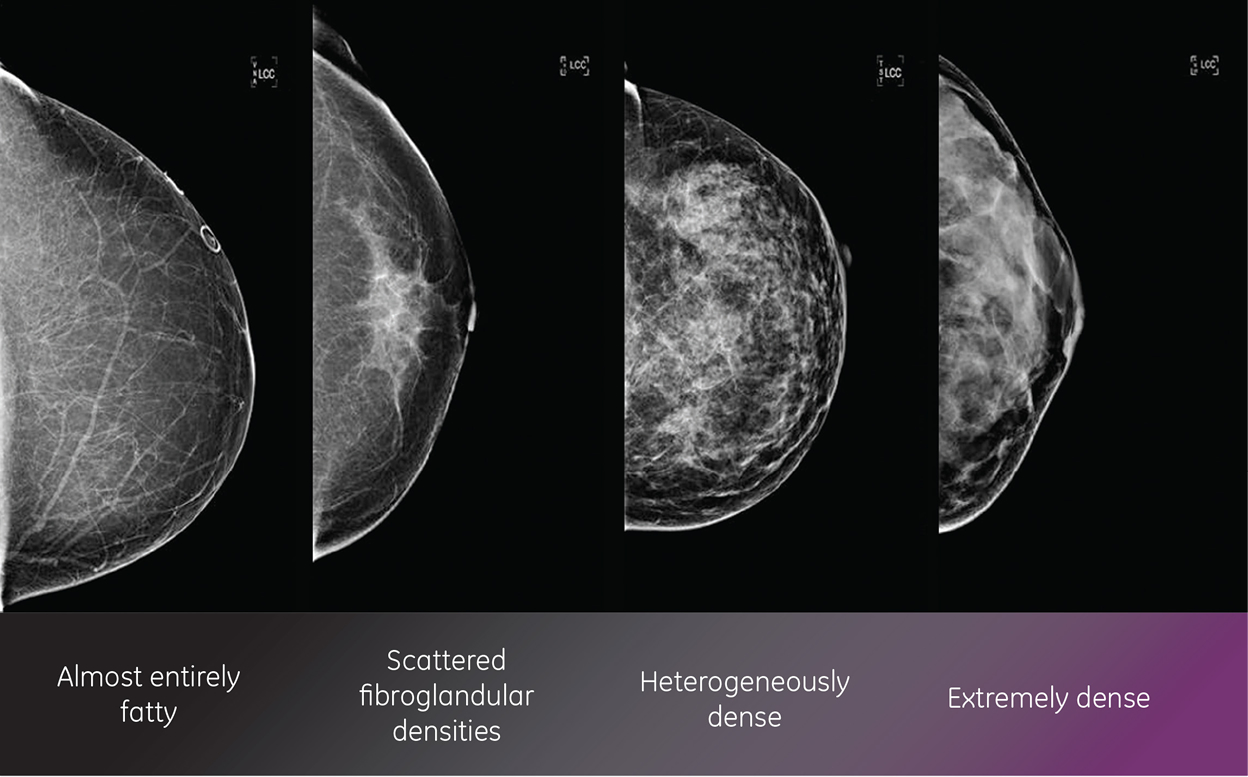
All breasts are not the same. Breasts are made out of fat and breast tissue. Some women have more fat than breast tissue while others have more breast tissue than fat.
At St. Luke’s, the advent of new breast screening technologies as well as an increased realization of mammography’s limitations in dense-breasted patients is ushering in a new era of personalized breast screening. Specifically, at St. Luke’s, the question we are now asking is, “What is the right screening test for each patient?”
“The mindset of, ‘If you have breasts, get a mammogram,’ is outdated,” says Dr. Russo. Individualized screening is the present and the future, because mammography may not be the best screening test for every woman, especially if you have dense breasts or a family history. Screening mammography remains a powerful life-saving tool in the hands of experienced breast radiologists and at high-volume diagnostic centers. Beyond that, however, we’ll soon experience a revolution in the way women’s breast health is achieved. The days where all women adhere to the same regimen of yearly mammography may be soon disappearing. At St. Luke’s, we’ve been ahead of the curve on this for quite a while already.”
What is the right screening test for each patient? “In answering this question,” says Dr. Russo, “we are taking into account a patient’s risk factors and breast density to determine whether screening ultrasound, breast MRI, or 3D mammography may serve as an effective supplement to mammography. A combination of carefully chosen screening exams may lead to a significant increase in cancer detection rate while decreasing the amount of unnecessary return visits and biopsies.”
Mammography is limited in sensitivity in women with dense breast tissue. Many women have dense breast tissue— in particular premenopausal women. Young women thought to be at high risk of breast cancer are often recommended to commence regular screening for breast cancer at 30 years of age. The dense breast tissue in these women makes detecting possible cancers difficult by x-ray mammography.
Standard ultrasound scans, using manual transducers, are commonly used in conjunction with mammography for many breast indications. Some studies have suggested that a combination of mammography and ultrasound may be more sensitive than mammography alone for detecting breast cancer in women with dense breasts, and ultrasound is commonly used to screen women with dense breasts, with or without the addition of mammograms and MRI. However, standard manual ultrasound is hampered by a lack of consistency across operators—the accuracy of manual ultrasound is highly dependent on the operator’s skill and experience. An automated ultrasound system may be able to overcome these limitations.
Dr. Russo compares a digital mammogram (left screen) to the automated breast ultrasound images of the same patient. With ABUS, he is able to not only view the breast from different angles, but can also view the various layers of breast tissue to find abnormalities.
“For women with dense breast tissue, mammography isn’t the best cancer detection tool,” says Dr. Russo. “It can be like trying to find a snowball in a snow storm. St. Luke’s new Automated Breast Ultrasound System (ABUS) is one of the newest technologies, providing an ultrasound of the entire breast; a uniform exam that’s relatively quick and easy to perform.” (See below for more detail on ABUS).
“Radiologists need to get more current and have a bigger arsenal of tools with which to screen for breast cancer, Dr. Russo says. “We’ve been doing breast MRI at St. Luke’s for a long time already, and it’s a good alternative to mammography. However, although MRI has good sensitivity for detecting breast cancer in dense breasts, it has a low specificity (high false-positive rate) and can be very expensive. And 3D mammography, right now, we believe has questionable clinical benefit; it currently delivers double the dose of radiation. We have a strong belief that the next generation of 3D mammography will be better, so we’re prudently holding out and waiting for it.”
A detailed mailing, including suggested flowcharts on how to order these various exams based on density and risk, as well as information on how to discuss this topic with patients, will soon be provided to referring clinicians.
“Our goal is to find more treatable breast cancers,” says Dr. Russo, “and we believe through our new personalized approach to breast screening that we’ll see a tremendous increase in cancer detection.”
Understanding the Breast Density Notification Act.
On Nov 21, 2013, Pennsylvania Governor Tom Corbett signed the Breast Density Notification Act into law. It requires mammography providers to notify women categorized as having dense breast tissue about their condition. Dense breast tissue can make it harder to find cancer on a mammogram and may be associated with an increased risk of cancer. The new law became effective January 31, 2014, and requires mammography providers to include the following language in letters sent to patients:
“This notice contains the results of your recent mammogram, including information about breast density. If your mammogram shows that your breast tissue is dense, you should know that dense breast tissue is a common finding and is not abnormal. Statistics show many women could have dense or highly dense breasts. Dense breast tissue can make it harder to find cancer on a mammogram and may be associated with an increased risk of cancer. This information about the result of your mammogram is given to you to raise your awareness and to inform your conversations with your physician. Together, you can decide which screening options are right for you, based on your mammogram results, individual risk factors or physical examination. A report of your results was sent to your physician.”
Pennsylvania is the 13th state to enact a breast density notification law.
Somo-v Automated Breast Ultrasound System (U-Systems, Inc.) for Breast Cancer Screening in Women with Dense Breast Tissue
The Somo-v® Automated Breast Ultrasound System (ABUS) (U-Systems, Inc., Sunnyvale, CA, USA) is intended to produce ultrasound images of the interior anatomy of the breast for breast cancer screening. The system consists of an integrated scanner, a computer, and a built-in workstation to view the images during acquisition. The entire system is mounted on wheels and is portable. The patient lies supine on a standard exam table. A technician applies a coupling gel to the breast and applies a film that compresses the breast tissue against the patient’s chest wall. The breast-shaped transducer is placed over the compressed breast. The ABUS system takes an automated scan of the entire breast and creates three-dimensional images of its structure. The images can be viewed on the built-in workstation or transferred to another workstation for analysis. Each breast exam is estimated to take 15 minutes to complete (including patient preparation), and the physician can review the images later.
ABUS
- Accurately detects small masses in dense breasts
- Automated process and positioning protocols enables rapid and reproducible exams, allowing for direct comparison with images obtained from a previous study
- Design of the transducer and patient’s supine position allow for maximal patient comfort
- Pattern-recognition software is user-friendly and allows a trained clinician to review a patient’s images in three minutes or fewer with a high degree of clinical confidence
- Noninvasive and does not expose the patient to radioactivity or contrast agents
St. Luke’s Regional Breast Center
Designated Breast Imaging Center of Excellence by American College of Radiology.
St. Luke’s Regional Breast Center, the first facility of its kind in the region to provide higher-level breast imaging exclusively, has been designated a Center of Excellence by the American College of Radiology.
Expert Staff Specially-Trained in Breast Health
In addition to providing the best digital imaging available today, the St. Luke’s Regional Breast Center has highly skilled technologists, breast health nurses and radiologists who are fellowship-trained in diagnostic mammography. The radiologists study images and provide verbal results during the appointment. In many cases, a same-day biopsy can be performed for the fastest possible results. The breast health nurses, who have special training in breast health, guide patients through every step of the diagnostic process. Women receive all the information they need to make good health care decisions in a timely fashion.
Featured Image: St. Luke’s ultrasonographer Jennifer Nytz performs a breast scan using ABUS at St. Luke’s Regional Breast Center in Center Valley.
View Dr. Russo’s Physician Video Profile.




